Clinical outcomes and repair integrity of arthroscopic rotator
4.9 (755) · $ 16.99 · In stock
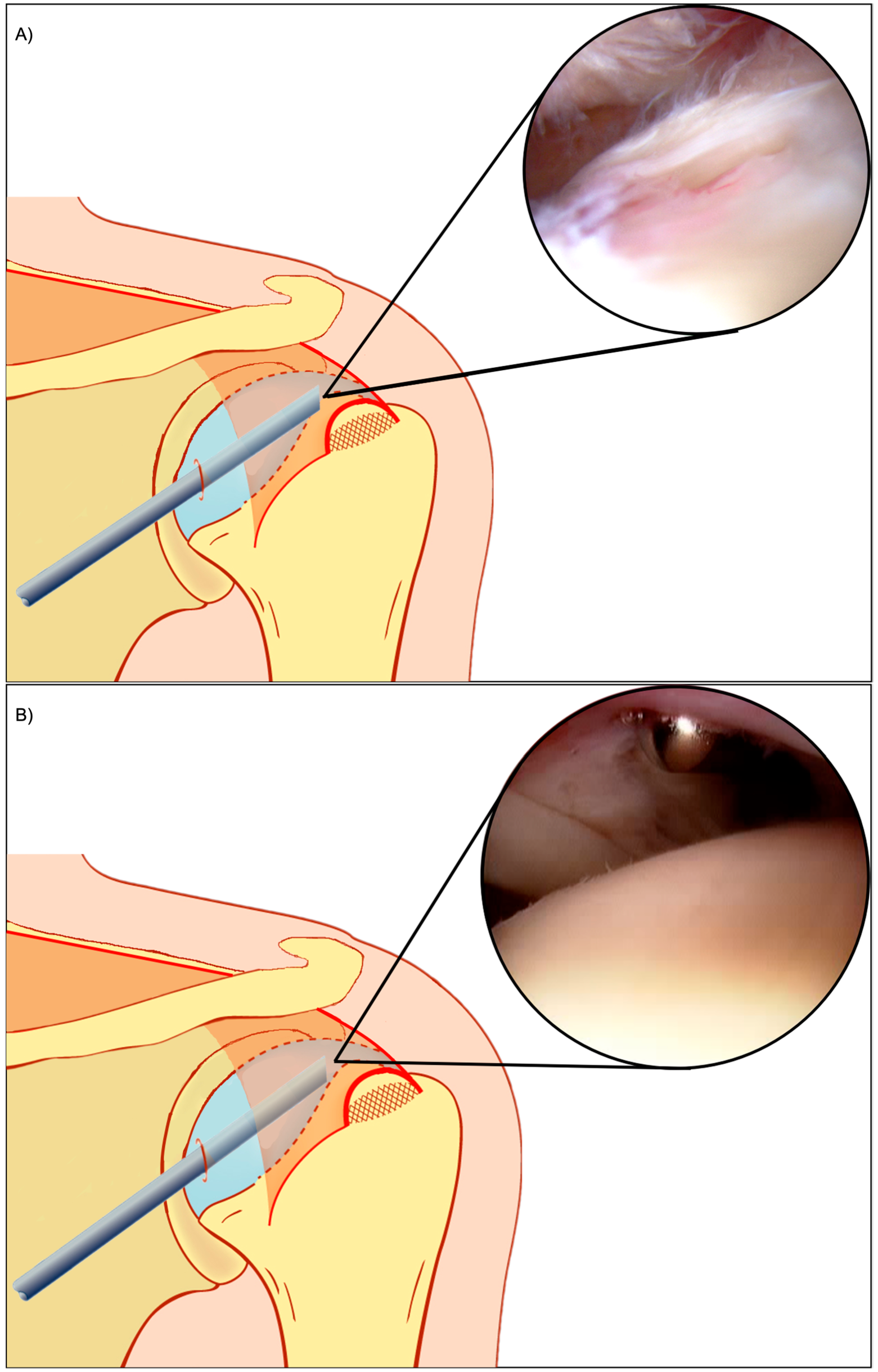
Background There have been few studies comparing clinical and radiological outcomes between the conventional and knotless suture-bridge techniques. The purpose of this study was to evaluate and compare the functional outcomes and repair integrity of arthroscopic conventional and knotless suture-bridge technique for full-thickness rotator cuff tears. Methods We prospectively followed 100 consecutive patients (100 shoulders) with full-thickness rotator cuff tears treated with the arthroscopic conventional or knotless suture-bridge technique from October 2012 to July 2014. Enrolled patients returned for follow-up functional evaluations at 1 and 2 years after the operation. There were four outcome measures in this study: American Shoulder and Elbow Surgeons (ASES) scores, Shoulder Rating Scale of the University of California at Los Angeles (UCLA) scores, Constant scores, and visual analog scale (VAS) pain scores. Enrolled patients returned for follow-up magnetic resonance imaging or ultrasonography evaluation to confirm the integrity of the repaired cuff at 6 months post-operation (97% follow-up rate). Also, we investigated the preoperative cuff retraction of enrolled patients using preoperative MRI to find out correlation between the stage of cuff retraction and re-tear rate. Results At final follow-up, the average UCLA, ASES, Constant, and VAS scores had improved significantly to 32.5, 88.0, 80.4, and 1.3, respectively, in the conventional suture-bridge technique group and to 33.0, 89.7, 81.2, and 1.2, respectively, in the knotless suture-bridge technique group. The UCLA, ASES, Constant, and VAS scores improved in both groups after surgery (all p < 0.001), and there were no significant differences between the two groups at 2-year follow-up (p = 0.292, 0.359, 0.709, and 0.636, respectively). The re-tear rate of repaired rotator cuffs was 16.3% (8/49 shoulders) in the conventional suture-bridge technique group and 29.2% (14/48 shoulders) in the knotless suture-bridge technique group; this difference was not significant (p = 0.131). There were no significant differences between the re-tear rate of the two groups in the Patte stage I and II (p = 0.358 and 0.616). Conclusions The knotless suture-bridge technique showed comparable functional outcomes to those of conventional suture-bridge techniques in medium-to-large, full-thickness rotator cuff tears at short-term follow-up. The knotless suture-bridge technique had a higher re-tear rate compared with conventional suture-bridge technique, although the difference was not significant.

Comparison of clinical outcome and repair integrity after arthroscopic suture-bridge and triple-row rotator cuff repairs of Fosbury flop tears - Journal of Orthopaedic Science

Medicina, Free Full-Text
JCM, Free Full-Text

The outcome and structural integrity of arthroscopic rotator cuff repair with use of the double-row suture anchor technique.

Relationship between hematoma-like tissue on the footprint and structural outcome of arthroscopic rotator cuff repair with a transosseous technique - JSES International

Short-term radiographic and clinical outcomes of arthroscopic rotator cuff repair with and without augmentation with an interpositional nanofiber scaffold

Patch augmentation does not provide better clinical outcomes than arthroscopic rotator cuff repair for large to massive rotator cuff tears

Clinical outcomes of arthroscopic superior capsule reconstruction in patients aged over 70 with irreparable rotator cuff tears - JSES International

The functional outcome of arthroscopic rotator cuff repair with double-row knotless vs knot-tying anchors

PDF) Repair integrity and clinical outcome after arthroscopic rotator cuff repair using single-row anchor fixation: A prospective study of single-tendon and two-tendon tears

Comparisons of Retear Patterns for 3 Arthroscopic Rotator Cuff Repair Methods

Short-term radiographic and clinical outcomes of arthroscopic rotator cuff repair with and without augmentation with an interpositional nanofiber scaffold